Coda Alliance, with Meghan Potthoff, Ph.D., developed the
Pediatric GoWish Together card game
to help parents navigate the unimaginable journey of their child’s illness.
Pediatric GoWish Together is a tool that provides parents a way to think and talk about what’s most important to them and their child. Becoming aware of these priorities empowers them to make decisions, facilitates communications with their medical team, solidifies family harmony, helps parents feel prepared to advocate for their child, and lessens their own uncertainties.
A Conversation Card Game for Parents and Pediatric Caregivers

Developed by Meghan Potthoff, PHD, APRN-NP, PPCNP-BC, CPNP-ACAssociate Professor, Lenke Family Scholar, Creighton University College of Nursing
In Collaboration with

Parents who’ve played Pediatric GoWish Together said
“This fog of medical terminology and words that we were living every day was so overwhelming that we didn’t even know what to ask. The cards gave me a focused point to organize my thoughts.”
Find out more about how Pediatric GoWish Together was developed
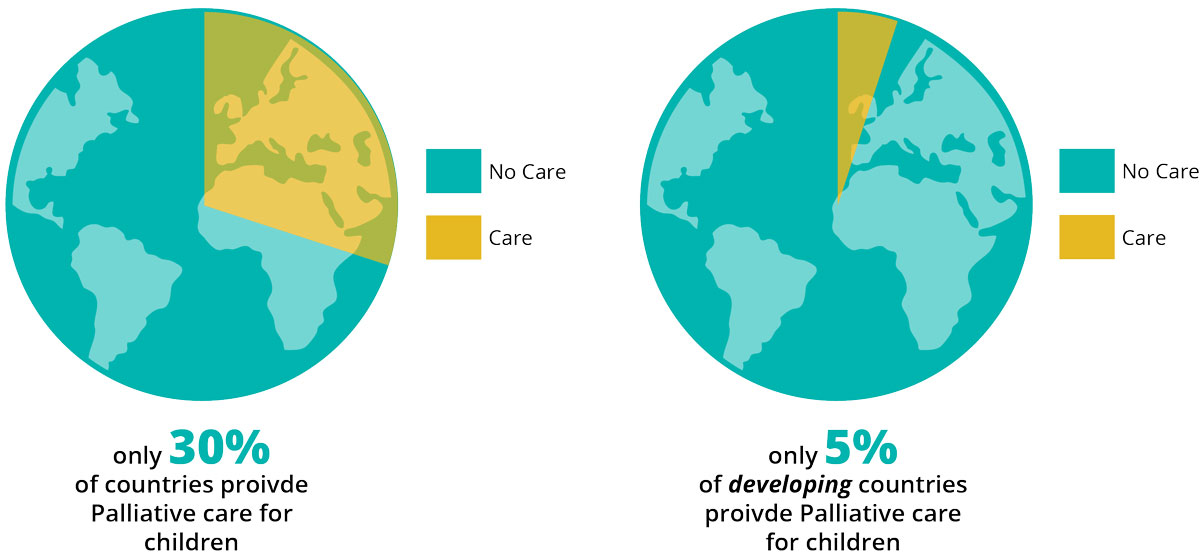
The International Children's Palliative Care Network (ICPCN) estimates that worldwide, twenty million children can benefit from palliative care.
How Pediatric GoWish Together helps you discover what’s important

Pediatric GoWish Together
A Conversation Game for Parents and Caregivers
We, at Coda Alliance, understand there’s nothing more difficult than facing end-of-life with your child or caring for a child with a life-threatening condition. Most parents experience the type of emotions that keep them from taking the actions needed to make things easier and more intuitive for their child, medical team, and family.
Understanding this and knowing how parents’ emotional difficulties deeply affect their child’s medical care, Dr. Meghan Potthoff joined with Coda to create a special set of their GoWish cards.
Coda’s Go-Wish cards, now used in 14 countries, have proven highly successful in helping people accept and begin end-of-life conversations. It provided the type of therapy the doctor was hoping for. So the connection was a natural next step for both.
The new Pediatric GoWish Together, A Conversation Game for Parents and Caregivers card game, was researched, tested, and revised by Megan Potthoff, Ph.D., Dr. Potthoff is an associate professor of nursing at Creighton University College of Nursing. And a Certified Advanced Pediatric Nurse Practitioner in Acute Care. She teaches pediatric nurse practitioner and research courses and is passionate about training strong clinicians who provide compassionate, high-level care to pediatric patients and their families.
She and Coda specifically designed the cards to help you navigate the stormy, unknown waters of a child’s illness. Dr. Potthoff’s research showed how the cards help to ease much of parents’ guilt and worry, as well as their unresolved sorrow and anger, and long-term uncertainty. How? By providing an easier way to start the conversation about end-of-life wishes.
Knowing your wishes empowers you to clear the fog, make decisions, and choose what’s right for your child’s healthcare. First, it’s both your right and your responsibility to help guide the medical team. And understanding each other’s wishes helps to put both parents, caregivers, and the medical team on the same page. With that, it solidifies family harmony, eases conversation with your child, and decreases the stress your child is feeling.
GoWish Pediatric GoWish Together is a sorting game with 41 cards, including a blank wish card. It’s topic to be determined by you. Each card offers suggestions as to what might be important to you, your child, and your family. What matters to you? How do you and your child wish to be treated? What important actions do you want to address? Ultimately, it’s up to you to choose what’s right for you and yours, but the cards help illuminate potential wishes you might consider.
A few suggestions you’ll find among the cards.
Do you wish?
- To minimize family arguments related to care decisions
- To identify and honor my child’s wishes
- To define the palliative care team’s role
It’s simple, all you need to do is sort the cards into three piles you label as very important, somewhat important, and not important. What’s most powerful, however, is discussing with your significant other why each chosen wish is important, or not important, to you. Then keep whittling down the cards to the top five or six cards that reflect what’s important to you.
Finally, share your chosen cards with your spouse, family, health care team, and your child.

How Pediatric GoWish Together was developed
Lighthouse in The Fog
By Meghan Potthoff, PhD.
Over the years, palliative care of children and families has become my passion. Because as a young nurse, I saw many deaths of children. In a lot of cases, we were trying to fit these children into an adult model of care, and it just wasn’t working very well. We needed new ideas and better models to fit the needs of the children and their families.
Research showed that common barriers identified by parents are all linked to ineffective, poor communication between the healthcare team and the family. We needed to finding means to improve conversations that help to alleviate some of these barriers identified by parents and improve outcomes for both the child and the parent throughout what’s known as, “The Pediatric Palliative Care Continuum. The continuum is a care model that conceptualizes the introduction of palliative care at the time of diagnosis and shows the synergy of combining curative treatment with supportive care. It reflects the needs of the pediatric patients suffering from chronic conditions that are life threatening but not necessarily terminal by definition.
I kept asking myself and my compatriots, how can we provide better services that reach greater numbers of people? How do we use altered models and technology to provide care particularly in underserved areas.
I decided to focus my doctoral research on developing an intervention to help parents verbalize their priorities. The card game called Go-Wish Pediatrics appeared to be the simplest and most engaging for parents to both use and benefit from. There’s a version for adults where they’re planning their own end-of-life goals. I modified the game with some parental involvement and tested it with parents in palliative care.
When we work with parents and ask them, “What do you need for the palliative care of your child,” they don’t know what to say. They don’t know what to ask for.
Hard conversations and decisions are an unfortunate reality for parents caring for children facing life threatening conditions. Confusing, inadequate, and inconsistent communication by health care providers makes advance care planning difficult in pediatrics.
But we found that by using this card game, which has about 50 prompts, parents are able to bring up questions they might feel uncomfortable or weird asking otherwise. Questions like: Am I weird to say that I’m worried about finances right now? Is that not appropriate to say when my child is going through this? Giving parents prompts gives them permission to say what their hopes, fears and priorities are. In a way, they can help manage their child’s palliative care.
One parent summed up what most parents of critically ill children feel:
“This fog of medical terminology and words that we were living every day was so overwhelming that we didn’t even know what to ask. The cards gave me a focused point to organize my thoughts.”
It’s exciting to have found a way to help families in a most difficult time.

Meghan R. Potthoff, PhD, APRN-NP
Associate Professor
Nursing
Dr. Meghan Potthoff is an associate professor of nursing at Creighton University College of Nursing. She teaches pediatric nurse practitioner and research courses and is passionate about training strong clinicians who provide compassionate, high-level care to pediatric patients and their families.
“I have centered my career and professional research around facilitating improved communication and family inclusion for pediatric patients suffering from life threatening or life limiting illness. I am committed to creating better palliative and end-of-life care for children and their families. To that end, I’ve worked with professionals at the Coda Alliance to develop a toolkit to guide conversations between health care professionals and the families of chronically ill children.” she said.
In 2020 Meghan Potthoff, PhD, received the honor of being one of 10 palliative care leaders accepted into the nationwide Sojourns Scholar Leadership Program.
Dr. Potthoff received her BSN from Creighton University, her MSN with a focus on pediatric acute care from the University of Pennsylvania and her PhD at South Dakota State University.
Her Current Research Focus
Pediatrics
Palliative Care
Obesity
Interprofessional Care

Pediatric GoWish Together FAQs
- What’s important to you, your child, and your family?
- What matters to you?
- How do you and your child wish to be treated?
- Is there anything you and your child would not want included in a treatment plan?


